

Not sleeping well or experiencing excessive daytime fatigue? Many common health conditions and medications can disrupt your sleep. Here’s how to spot if a medical cause is keeping you up at night.

Adapted with permission from Improving Sleep: A Guide to a Good Night’s Rest, a special health report published by Harvard Health Publishing.
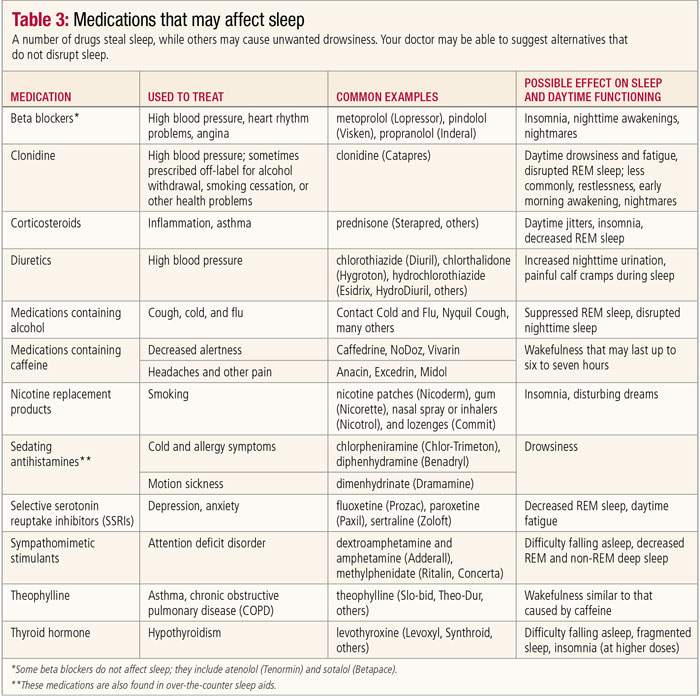
People who feel they sleep perfectly well may still be troubled by excessive daytime sleepiness because of a variety of underlying medical illnesses. A sleep disturbance may be a symptom of a health issue or an adverse effect of therapy to treat the problem. The stress of chronic illness can also cause insomnia and daytime drowsiness. Common conditions often associated with sleep problems include heartburn, diabetes, cardiovascular disease, musculoskeletal disorders, kidney disease, mental health problems, neurological disorders, respiratory problems, and thyroid disease. In addition, a number of prescription and over-the-counter medications used to treat these and other health problems can impair sleep quality and quantity (see table below).
Lying down in bed often worsens heartburn, which is caused by the backup of stomach acid into the esophagus. You may be able to avoid this problem by abstaining from heavy or fatty foods—as well as coffee and alcohol—in the evening. You can also use gravity to your advantage by elevating your upper body with an under-mattress wedge or blocks placed under the bedposts. Over-the-counter and prescription drugs that suppress stomach acid secretion can also help.
Diabetes is a common, chronic disorder marked by elevated levels of blood glucose, or sugar. It occurs when your cells don’t respond appropriately to insulin (a hormone secreted by the pancreas), and when your pancreas can’t produce more insulin in response. People with diabetes whose blood sugar levels are not well controlled may experience sleep problems due to:
If diabetes has damaged nerves in the legs, nighttime movements or pain may also disturb sleep.
Heart failure is a condition characterized by a gradual decline in the heart’s ability to “pump”, or circulate blood adequately. Heart failure can cause fluid to build up in the lungs and tissues. Patients with heart failure may awaken during the night feeling short of breath because extra body fluid accumulates around their lungs when they’re lying down. Using pillows to elevate the upper body may help. These people can also be awakened just as they are falling asleep by a characteristic breathing pattern called Cheyne-Stokes respiration, a series of increasingly deep breaths followed by a brief cessation of breathing.
Benzodiazepine sleep medications help some people to stay asleep despite this breathing disturbance, but others may need to use supplementary oxygen or a device that increases pressure in the upper airway and chest cavity to help them breathe and sleep more normally.
Men with heart failure frequently have obstructive sleep apnea—a breathing disorder characterized by multiple nighttime awakenings—which can disrupt sleep, cause daytime sleepiness, and worsen heart failure. In people with coronary artery disease, the natural fluctuations in circadian rhythms may trigger angina (chest pain), arrhythmia (irregular heartbeat), or even heart attack while asleep.
Arthritis pain can make it hard for people to fall asleep and to resettle when they shift positions. In addition, treatment with steroids frequently causes insomnia. You may find it helpful to take aspirin or a nonsteroidal anti-inflammatory drug (NSAID) just before bedtime to relieve pain and swelling in your joints during the night.
[Read: Chronic Pain and Mental Health]
People with fibromyalgia—a condition characterized by painful ligaments and tendons—are likely to wake in the morning still feeling fatigued and as stiff and achy as a person with arthritis. Researchers who analyzed the sleep of fibromyalgia sufferers have found that at least half have abnormal deep sleep, in which slow brain waves are mixed with waves usually associated with relaxed wakefulness, a pattern called alpha-delta sleep.
People with kidney disease have kidneys that are damaged to the extent that they can no longer filter fluids, remove wastes, and keep electrolytes in balance as efficiently as they did when healthy. Kidney disease can cause waste products to build up in the blood and can result in insomnia or symptoms of restless legs syndrome. Although researchers aren’t sure why, kidney dialysis or transplant does not always return sleep to normal.
Nocturia is the need to get up frequently to urinate during the night. It is a common cause of sleep loss, especially among older adults. A mild case causes a person to wake up at least twice during the night; in severe cases, a person may get up as many as five or six times.
Nocturia may be a product of age, but other causes include certain medical conditions (heart failure, diabetes, urinary tract infection, an enlarged prostate, liver failure, multiple sclerosis, sleep apnea), medication (especially diuretics), and excessive fluid intake after dinner.
Therapies for nocturia fall into three categories:
The first step is to try to identify the cause and correct it. If this is unsuccessful, try behavioral
approaches such as cutting down on how much you drink in the two hours before bedtime, especially caffeine and alcohol. If the nocturia persists, your doctor may prescribe one of a growing number of medications approved to treat an overactive bladder.
An overactive thyroid gland (hyperthyroidism) can cause sleep problems. The disorder overstimulates the nervous system, making it hard to fall asleep, and it may cause night sweats, leading to nighttime arousals. Feeling cold and sleepy is a hallmark of an underactive thyroid (hypothyroidism).
Because thyroid function affects every organ and system in the body, the symptoms can be wide-ranging and sometimes difficult to decipher. Checking thyroid function requires only a simple blood test, so if you notice a variety of unexplained symptoms, ask your doctor for a thyroid test.
Circadian-related changes in the tone of the muscles surrounding the airways can cause the airways to constrict during the night, raising the potential for nocturnal asthma attacks that rouse the sleeper abruptly.
Breathing difficulties or fear of having an attack may make it more difficult to fall asleep, as can the use of steroids or other breathing medications that also have a stimulating effect, similar to that of caffeine.
People who have emphysema or bronchitis may also have difficulty falling and staying asleep because of excess sputum production, shortness of breath, and coughing.
Almost all people with anxiety or depression have trouble falling asleep and staying asleep. In turn, not being able to sleep may become a focus of some sufferers’ ongoing fear and tension, causing further sleep loss.
Severe anxiety, also known as generalized anxiety disorder, is characterized by persistent, nagging feelings of worry, apprehension, or uneasiness. These feelings are either unusually intense or out of proportion to the real troubles and dangers of the person’s everyday life.
People with general anxiety typically experience excessive, persistent worry every day or almost every day for a period of six months or more. Common symptoms include trouble falling asleep, trouble staying asleep, and not feeling rested after sleep.
Phobias, which are intense fears related to a specific object or situation, rarely cause sleep problems unless the phobia is itself sleep-related (such as fear of nightmares or of the bedroom). Panic attacks, on the other hand, often strike at night. In fact, the timing of nocturnal attacks helped convince psychiatrists that these episodes are biologically based.
Sleep-related panic attacks do not occur during dreaming, but rather in stage N2 (light sleep) and stage N3 (deep sleep), which are free of psychological triggers. In many phobias and panic disorders, recognizing and treating the underlying problem—often with an anti-anxiety medication—may solve the sleep disturbance.
Because almost 90% of people with serious depression experience insomnia, a physician evaluating a person with insomnia will consider depression as a possible cause. Waking up too early in the morning is a hallmark of depression, and some depressed people have difficulty falling asleep or get fitful sleep throughout the whole night.
In chronic, low-grade depression (also known as dysthymia), insomnia or sleepiness may be the most prominent symptom. Laboratory studies have shown that people who are depressed spend less time in slow-wave sleep and may enter REM sleep more quickly at the beginning of the night.
Disturbed sleep is a prominent feature of bipolar disorder (also known as manic-depressive illness). Sleep loss may exacerbate or induce manic symptoms or temporarily alleviate depression. During a manic episode, a person may not sleep at all for several days. Such occurrences are often followed by a “crash” during which the person spends most of the next few days in bed.
Some people with schizophrenia sleep very little in the early, most severe stage of an episode. Between episodes, their sleep patterns are likely to improve, although many people with schizophrenia rarely obtain a normal amount of deep sleep.
Certain brain and nerve disorders can contribute to sleeplessness.
Alzheimer’s disease and other forms of dementia may disrupt sleep regulation and other brain functions. Wandering, disorientation, and agitation during the evening and night, a phenomenon known as “sundowning,” can require constant supervision and place great stress on caregivers. In such cases, small doses of antipsychotic medications are more helpful than benzodiazepine drugs.
People with epilepsy—a condition in which a person is prone to seizures—are twice as likely as others to suffer from insomnia. Brain wave disturbances that cause seizures can also cause deficits in slow-wave sleep or REM sleep. Antiseizure drugs can cause similar changes at first, but tend to correct these sleep disturbances when used for a long time.
About one in four people with epilepsy has seizures that occur mainly at night, causing disturbed sleep and daytime sleepiness. Sleep deprivation can also trigger a seizure, a phenomenon noted in college infirmaries during exam periods, as some students suffer their first seizures after staying up late to study.
People who are prone to headaches should try to avoid sleep deprivation, as lack of sleep can promote headaches. Both cluster headaches and migraines may be related to changes in the size of blood vessels leading to the cortex of the brain; pain occurs when the walls of the blood vessels dilate.
Researchers theorize that as the body catches up on missed sleep, it spends more time in delta sleep, when vessels are most constricted, making the transition to REM sleep more dramatic and likely to induce a headache. Headaches that awaken people are often migraines, but some migraines can be relieved by sleep. Sleepiness coupled with dizziness, weakness, headache, or vision problems may signal a serious problem such as a brain tumor or stroke, which requires immediate medical attention.
Almost all people with Parkinson’s disease have insomnia. Just getting in and out of bed can be a struggle, and the disease often disrupts sleep. Some arousals are from the tremors and movements caused by the disorder, and others seem to result from the disorder itself. As a result, daytime sleepiness is common.
Treatment with sleeping pills may be difficult because some drugs can worsen Parkinson’s symptoms. Some patients who take drugs used to treat Parkinson’s treatment may develop severe nightmares; others experience disruption of REM sleep. However, the use of these medications at night is important to maintain the mobility needed to change positions in bed. A bed rail or an overhead bar (known as a trapeze) may make it easier for people with Parkinson’s to move about and, therefore, lead to better sleep.
Adapted with permission from Improving Sleep: A Guide to a Good Night’s Rest, a special health report published by Harvard Health Publishing.
Last updated or reviewed on February 23, 2023Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
Donate to HelpGuide.org today